There are some components of neurological examination:-
1.Assessing Consciousness and Cognition
2.Examination of cranial Nerves
3.Examining the motor System
4. Examining the Sensory System
5. Examining the reflexes
ASSESSSING CONCIOUSNESS AND COGNITION :-
Cerebral abnormalities may cause disturbances in mental status, intellectual functioning, thought content, and emotional status.
The examiner records and reports specific observations regarding mental status, intellectual function, thought content, and emotional status all of which permits comparison by others over time.
Analysis and the conclusions that may be drawn from these findings usually depend on the examiner's knowledge of neuroanatomy, neurophysiology, and neuropathology.
1. Mental status :- An assessment of mental status begins by observing the patients appearance and behaviour, noting dress, grooming, and personal hygiene. Posture ,gestures, movements and facial expressions often provide important information about the patient.
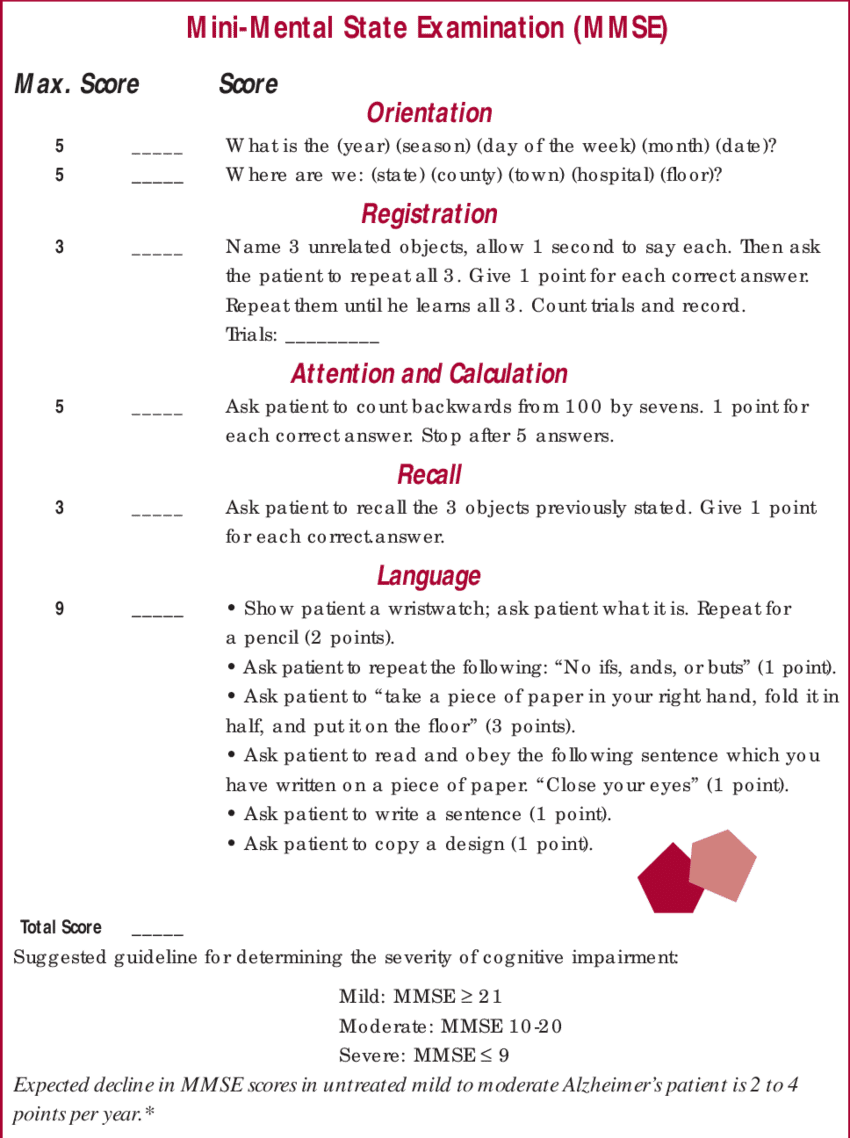
2. Intellectual Function :- A person with an average intelligence quotient(IQ) can repeat seven digits without faltering and can recite five digits backward.
The examiner might ask the patient to count backward from 100 Or to subtract 7 from 100, then 7 from that, and so fourth(referred to as serial 7s) .
3. Thought content :- During the interviews, it is important to assess the patients thought content. Are the patients thoughts spontaneous, natural, clear, relevant, and coherent? Does the patients have any fixed ideas, illusions, or preoccupations?
4.Emotional status :- An assessment of consciousness and cognition also includes the patient's emotional status. Is the patient's affect natural and even, or irritable and angry, anxious, apathetic or flat, or euphoric? Does his or her mood fluctuate normally or does the patients unpredictably swing from joy to sadness during the interview?
5. Language ability :- The person with normal neurologic function can understand and communicate in spoken and written language. Does the patient answer questions appropriately? Can he or she read a sentence from a newspaper and explain its meaning?
6.Impact on lifestyle :-
The nurse assesses the impact of any impairment on the patients lifestyle. Issues to consider include the limitations imposed on the patient by any cognitive deficit and the patient's role in society, including family and community roles.
The plan of care that the nurse develops needs to address and support adaptation to the neurologic deficit and continued function to the extent possible within the patients support system.
7.Level of Consciousness :-
Consciousness is the patients wakefulness and ability to resond to the environment. Level of consciousness is the most sensitive indicator of neurologic function. The assess level of consciousness, the examiner observes for alertness and ability to follow commands.
EXAMINING OF CRANIAL NERVES
Cranial nerves are assessed when level of consciousness is decreased, with brain stem pathology, or in the presence of peripheral nervous system disease.
Equipment for assessing cranial nerve function :-
1.Tongue depressor
2. Flashlight
3. Sugar and salt samples
4. Watch
5. Cotton tipped swab
6.cotton swabs
7.Snellen chart
8. Ophthalmoscope
9. Samples of familiar odors
10. Tuning forks
11. Tubes of hot and cold water

EXAMINING THE MOTOR SYSTEM
* Motor ability:-A thorough examination of the motor system includes an assessment of muscles size and tone as well as strength, coordination, and balance.
The patients instructed to walk across the room, if possible, while examiner observes posture and gait.
The muscles are inspected and palpated if necessary, for their size and symmetry.
Abnormalities in tone include Spasticity (increase muscle tone), rigidity (resistance to passive strecth), and flaccidity.
*Muscle strength :- Assessing the patients ability to flex or extend the extremities against resistance tests muscle strength.
The quadriceps, for example:- is a powerful muscle responsible for straightening the legs. Once the legs is straightended, it is exceedingly difficult for the examiner to flex the knee. If the knee is flexed and the patient is asked to straighthen the leg against resistance, weakness can be elicited.
Clinicians use 5 point scale to rate muscle strength:-
*Balance and coordination:-
Cerebellar and basal ganglia influence on the motor system is reflected in balance control and coordination.
The Romberg test is a screening test for balance that can be done with the patients seated or standing The patients can be seated or stand with feet together and arms at the side, first with eye 👀 open and then with both eyes closed for 20 seconds.
The examiner stands close to support the standing patients if he or she begins to fall.
Slight swaying is normal, but a loss of balance is abnormal and is considered a positive Romberg Test.
Additional cerebral tests for balance in ambulatory patients include hopping in place, alternating knee bends, and heel -to - toe walking (both forward and backward).
Coordination in the hands and upper extremities is tested by having the patients perform rapid, alternating movements and point -to-point testing.
Coordination in the lower extremities is tested by having the patients run the heel down the anterior surface of the tibia of the other leg. Each leg tested in turn.
Ataxia is an incoordination of voluntary muscle action, particularly of the muscle groups used in activities such as walking and reaching for objects.
EXAMINING OF SENSORY SYSTEM
The sensory system is even more complex then the motor system, because sensory modalities are more widespread through out the central and peripheral nervous system.
Assessment of sensory systems involves
* Tests for tactile sensation
* superficial pain
* Temperature
* Vibration
* Position sense (proprioception).
1.Tactile sensation is assessed by lightly touching a cotton wisp or fingertip to corresponding area on each side of the body.
2.Pain and temperatures sensations are transmitted together in lateral part of the spinal cord, so it is unnecessary to test for temperature sense in most circumstances.
Determining patients sensitivity to a sharp objects can assess superficial pain perception.
3.vibration and proprioception are transmitted together in the posterior part if the cord. Vibration may be evaluated through the use of a low- frequency (128-256Hertz [Hz]) tuning fork. The handle of the vibrating fork is placed against a bony prominence and the patient is asked if he or she feels a sensation and is instructed to signal the examiner when the sensation ceases.
Common locations used to test for vibratory sense include the distal joint of the great toe and the proximal thumb joint.
4.position or sense of proprioception may be determined by asking the patient to close both eyes and indicate, as the great toe or index finger alternatively moved up and down, in which direction movement has taken place. Vibration and position sense are often lost together, frequently in circumstances in which all other sensation remains intact.
EXAMINING THE REFLEXES
Reflexes are involuntary contractions of muscles and muscle groups in response to a stimulus. Testing reflexes enables the examiner to assess involuntary reflex arcs that depends on the presence of afferent stretch receptors, spinal and brain stem synapses, efferent motor fibers, and a variety of modifying influences from higher level.
There are some reflexes
1.Biceps Reflex:- The biceps reflex is elicited by striking the biceps tendon over a slightly flexed elbow. The examiner supports the forearm at the tendon and striking the thumb with the reflexe hammer. The normal response is flexion at the elbow and contractions of the biceps.
2. Triceps Reflex :- To elicit a triceps reflex, the patients arm is flexed at the elbow and hanging freely at the side. The examiner supports the patients arm and identifies the triceps tendon by palpating 2.5 to 5 cm above the elbow. A direct blow on the tendon normally produces contraction of the triceps muscle and extension of the elbow.
3. Brachioradialis Reflex :- with the patients forearm resting on the lap ir across the abdomen, the brachioradialis reflex is assessed. A gentle strike of the hammer 2.5 to 5 cm above the wrist results in flexion and supination of the forearm.
4. Patellar Reflex :- The patellar reflex is elicited by striking the patellar tendon just below the patella. The patients may be in a sitting or a lying position. If the patients is supine, the examiner supports the legs to facilitate relaxation of the muscles.
Contractions of the quadriceps ans knee extension are normal response.
5. Achilles Reflex :- To elicit an Achilles reflex, the foot is dorsiflexed at the ankle and the hammer strikes the stretched Achilles tendon. This reflex normally produces planter flexion. If the examiner cannot relax, the patient is instructed to kneel on a chair or similar evaluated flat surface.

















0 Comments